Outcomes of Different Wound Dressings and Offloading Combinations in Diabetic Foot Ulcers: A Systematic Review
Wound dressings & Offloading in DFU
Abstract
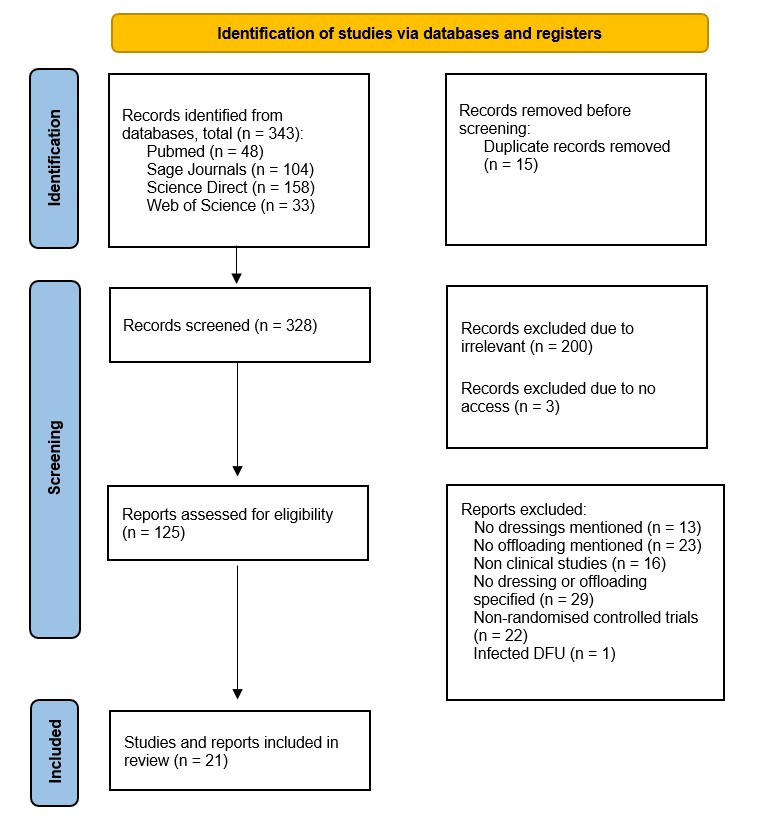
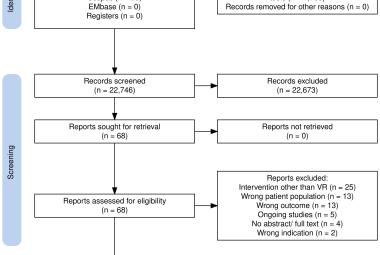
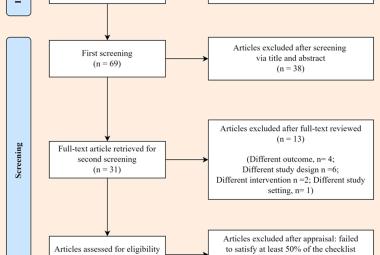
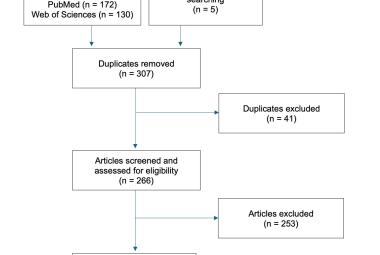
Both wound dressings and offloading are important in managing diabetic foot ulcer (DFU). However previous systematic reviews only evaluate the effectiveness of each intervention separately. Therefore, we would like to provide an insight of the combined effectiveness of both wound dressing and offloading techniques. This systematic review is carried out in compliance with the Preferred Reporting in Systematic Reviews and Meta-Analyses (PRISMA) and was registered to PROSPERO (registration number: CRD42024624203) prior to starting the review. Four databases were utilised for the review: PubMed, ScienceDirect, Sage Journals and Web of Science. Keywords included “diabetic foot ulcer”, “wound dressing” and “offloading”. Randomised controlled trials between 2015 to 2024 that specified the type of dressing and type of offloading were included. Data extraction focused on the type of dressings, offloading and healing outcomes of DFUs. 21 studies were included. All studies showed that the combination of dressing and offloading created good healing outcomes in terms of healing time, reduction in wound size and other factors such as quality of life. The highest rate of complete healing (90%) was achieved by using silver hydrogel and orthotic shoes; while the shortest healing time was achieved by using honey and hydrogel alternatively with orthotic shoes (p=0.004). It is clear that the combination of wound dressings together with offloading positively impacts the healing process of DFU. However, as the clinical heterogeneity limitations such as different mean ulcer sizes, number of patients, it is hard to determine the best combination of dressings and offloading.
Keywords :
Diabetic foot ulcer; offloading; wound dressings,
Abstrak
Kedua-dua pembalut luka dan pemunggahan adalah penting dalam menguruskan ulser kaki diabetik (DFU). Namun, kajian sistematik yang wujud hanya menilai keberkesanan kedua-dua intervensi secara berasingan. Oleh itu, kajian ini bertujuan untuk memberikan gambaran tentang keberkesanan gabungan antara kedua-dua teknik pembalut luka dan pemunggahan. Kajian sistematik ini dijalankan selaras dengan garis panduan Preferred Reporting in Systematic Reviews and Meta-Analyses (PRISMA) dan telah didaftarkan di PROSPERO (nombor pendaftaran: CRD42024624203) sebelum kajian dimulakan. Empat pangkalan data telah digunakan iaitu PubMed, ScienceDirect, Sage Journal dan Web of Science. Kata kunci yang digunakan termasuk “diabetic foot ulcer”, "wound dressing" dan “offloading”. Kajian terkawal rawak yang diterbitkan antara tahun 2015 hingga 2024 yang menyatakan jenis pembalut luka dan jenis pemunggahan telah dirangkumkan dalam kajian ini. Pengekstrakan data memberi tumpuan kepada jenis pembalut luka, kaedah pemunggahan dan hasil penyembuhan DFU. Sebanyak 21 kajian telah dirangkumkan. Semua kajian menunjukkan bahawa gabungan pembalut luka dan pemunggahan menghasilkan hasil penyembuhan yang baik dari segi masa penyembuhan, pengurangan saiz luka serta faktor lain seperti kualiti hidup. Kadar penyembuhan lengkap tertinggi (90%) dicapai melalui penggunaan hidrogel perak dan kasut ortotik; manakala masa penyembuhan paling singkat dicapai melalui penggunaan madu dan hidrogel secara alternatif bersama kasut ortotik (p = 0.004). Secara keseluruhan, gabungan pembalut luka dan pemunggahan memberi kesan positif kepada proses penyembuhan DFU. Walau bagaimanapun, batasan heterogeniti klinikal seperti perbezaan purata saiz ulser dan bilangan pesakit menyebabkan kesukaran untuk menentukan kombinasi terbaik pembalut luka dan pemunggahan yang paling berkesan.
Kata Kunci :
Pemunggahan; teknik pembalut luka; ulser kaki diabetik,
Correspondance Address
Chan Junji. Tissue Engineering Group (TEG), National Orthopaedic Centre of Excellence for Research and Learning, Department of Orthopaedic Surgery, Faculty of Medicine, Universiti Malaya, Kuala Lumpur 50603, Malaysia. Tel: +6012 2860526 Email: popcccc2022@gmail.com